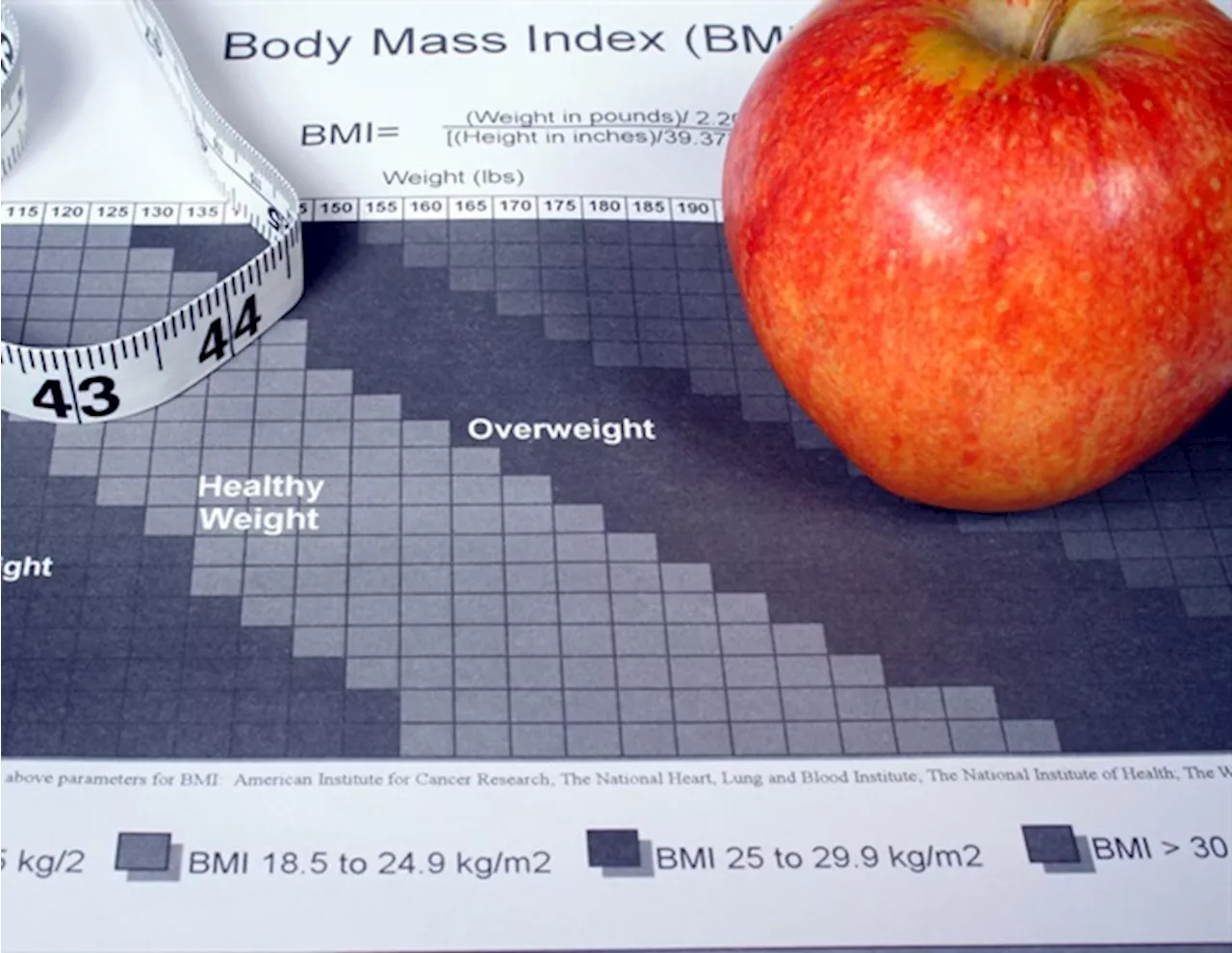
A nerve-stimulation treatment for obstructive sleep apnea that originally was approved only for people with body mass indexes (BMIs) in the healthy range recently was extended to patients with BMIs up to 40, a weight range generally described as severely obese.
Apr 4 2024Washington University School of Medicine A nerve-stimulation treatment for obstructive sleep apnea that originally was approved only for people with body mass indexes in the healthy range recently was extended to patients with BMIs up to 40, a weight range generally described as severely obese. A healthy BMI ranges from 18.5 to 24.9.
Our study shows that the more overweight you are, the less likely it is that nerve-stimulation treatment will be effective in treating your sleep apnea." "I'm not saying that we shouldn't put this device in patients with a BMI of 38 or 40. But my job as a physician is to help overweight patients make an informed decision, to better understand their odds of success and realize that the chances of it working for them may be a lot less.
To many patients, hypoglossal nerve stimulation looks like an appealing alternative to CPAP machines. The therapy is driven by a small, battery-operated device implanted just above the ribs. A small wire is run internally up the chest and into the jaw, where it connects to the hypoglossal, a nerve that controls tongue muscles responsible for keeping the upper airway open during sleep.
Landsness, a sleep researcher who treats patients with sleep apnea, was surprised by the changes in the eligibility criteria. To understand how the device performs in people of varying sizes, he and colleagues performed an independent evaluation using data from 78 people with BMIs up to 35 who received implants of the nerve-stimulation device at the Washington University Sleep Medicine Center from 2019 through 2023.
"Body mass index is clearly an important factor in predicting whether hypoglossal nerve stimulation will work for an individual patient," Landsness said. "Our study shows an almost linear relationship between BMI and treatment success. For every unit of BMI increase over 32, the odds of successful treatment decrease by about 17%."
Sleep Apnea Body Mass Index Breathing Medicine Neck Nerve Neurology Obstructive Sleep Apnea Otolaryngology Research Surgery Tongue
United States Latest News, United States Headlines
Similar News:You can also read news stories similar to this one that we have collected from other news sources.
 Nerve stimulation for sleep apnea found to be less effective for people with higher BMIsA nerve-stimulation treatment for obstructive sleep apnea that originally was approved only for people with body mass indexes (BMIs) in the healthy range recently was extended to patients with BMIs up to 40, a weight range generally described as severely obese. A healthy BMI ranges from 18.5 to 24.9.
Nerve stimulation for sleep apnea found to be less effective for people with higher BMIsA nerve-stimulation treatment for obstructive sleep apnea that originally was approved only for people with body mass indexes (BMIs) in the healthy range recently was extended to patients with BMIs up to 40, a weight range generally described as severely obese. A healthy BMI ranges from 18.5 to 24.9.
Read more »
 Higher BMI variability linked to adverse cardiovascular disease eventsHigher body mass index (BMI) variability is associated with adverse cardiovascular disease (CVD) events, according to a study published online March 21 in JAMA Network Open.
Higher BMI variability linked to adverse cardiovascular disease eventsHigher body mass index (BMI) variability is associated with adverse cardiovascular disease (CVD) events, according to a study published online March 21 in JAMA Network Open.
Read more »
 Childhood BMI tied to higher blood pressure in middle ageChildren and teenagers living with overweight or obesity are more likely to have high blood pressure as adults (aged 50-64 years), suggesting the processes behind the condition could begin as early as childhood, suggests new research being presented at this year's European Congress on Obesity (ECO) in Venice, Italy (12-15 May).
Childhood BMI tied to higher blood pressure in middle ageChildren and teenagers living with overweight or obesity are more likely to have high blood pressure as adults (aged 50-64 years), suggesting the processes behind the condition could begin as early as childhood, suggests new research being presented at this year's European Congress on Obesity (ECO) in Venice, Italy (12-15 May).
Read more »
 Overweight children ‘more likely to have high blood pressure as adults’, study suggestsStudy shows blood pressure in adult men increased in line with higher childhood BMI and greater BMI change during puberty
Overweight children ‘more likely to have high blood pressure as adults’, study suggestsStudy shows blood pressure in adult men increased in line with higher childhood BMI and greater BMI change during puberty
Read more »
 Study reveals obesity's link to increased risk of multiple sclerosis and ischemic strokeThe genetic relationship between body mass index (BMI) and multiple neurological diseases.
Study reveals obesity's link to increased risk of multiple sclerosis and ischemic strokeThe genetic relationship between body mass index (BMI) and multiple neurological diseases.
Read more »
 Overweight primary school girls more likely to seek doctor's help for musculoskeletal problemsPrimary school girls between the ages of 4 and 11 with a body mass index (BMI) considered overweight or obese are more likely to see a family doctor (GP) at least once about musculoskeletal problems than their healthy weight peers, suggests research, focused on one area of London and published online in the Archives of Disease in Childhood.
Overweight primary school girls more likely to seek doctor's help for musculoskeletal problemsPrimary school girls between the ages of 4 and 11 with a body mass index (BMI) considered overweight or obese are more likely to see a family doctor (GP) at least once about musculoskeletal problems than their healthy weight peers, suggests research, focused on one area of London and published online in the Archives of Disease in Childhood.
Read more »
