Waiting to deliver insulin until the patient has eaten at least half of their meal reduced hypoglycemia without raising severe hyperglycemia.
In a single-center study, shifting the timing of nutritional insulin from pre- to post-prandial reduced the risk for hypoglycemia without affecting rates of severe hyperglycemia or hospital length of stay.The retrospective study performed at a community hospital evaluated adult inpatients receiving nutritional insulin.
On June 28, 2019, hospital policy changed the timing of nutritional insulin from preprandial to administration after at least 50% of the meal was consumed. Analysis stratified by three time periods: Preintervention, September 2018 to June 27, 2019; immediate postintervention, July 2019 to February 2020; and distant postintervention, September 2022 to August 2023).
Outcomes included rates of hypoglycemia , moderate hypoglycemia , severe hypoglycemia , severe hyperglycemia , daily mean glucose, and length of stay . The number of patient-days analyzed for timepoints 1, 2, and 3 were 1948, 1751, and 3244 patient-days, respectively.Unadjusted rates of any hypoglycemia were significantly reduced across the three time periods, from 9.4% to 8.9% to 6.7% , but not between timepoints 1 and 2.=.24), while there was a nonsignificant trend toward lower severe hypoglycemia rates , although mean daily glucose did significantly increase over time , but not between 1 and 2.
Hospitals Hyperglycemia Inpatient Care Inpatient Hemoglobin A1c Hemoglobin A1c Test Glycated Hemoglobin Glycosylated Hemoglobin Hba1c A1C Hb1c Glycohemoglobin Ghb Diabetic Control Index A1C Assay
United States Latest News, United States Headlines
Similar News:You can also read news stories similar to this one that we have collected from other news sources.
 How blockbuster obesity drugs create a full feeling — even before one bite of foodScientists identify brain area harbouring two groups of neurons: one for pre-meal sensations of fullness, and one for post-meal satiety. Scientists identify brain area that holds two groups of neurons: one for pre-meal sensations of fullness and one for post-meal satiety.
How blockbuster obesity drugs create a full feeling — even before one bite of foodScientists identify brain area harbouring two groups of neurons: one for pre-meal sensations of fullness, and one for post-meal satiety. Scientists identify brain area that holds two groups of neurons: one for pre-meal sensations of fullness and one for post-meal satiety.
Read more »
 Proteins and fats can drive insulin production for some, paving way for tailored nutritionWhen it comes to managing blood sugar levels, most people think about counting carbs. But new research shows that, for some, it may be just as important to consider the proteins and fats in their diet.
Proteins and fats can drive insulin production for some, paving way for tailored nutritionWhen it comes to managing blood sugar levels, most people think about counting carbs. But new research shows that, for some, it may be just as important to consider the proteins and fats in their diet.
Read more »
 Hypoglycemia Risk Limits Use of Once-Weekly Insulin in T1DDr Anne Peters discusses the risk for hypoglycemia with the use of once-weekly insulin icodec in patients with type 1 diabetes.
Hypoglycemia Risk Limits Use of Once-Weekly Insulin in T1DDr Anne Peters discusses the risk for hypoglycemia with the use of once-weekly insulin icodec in patients with type 1 diabetes.
Read more »
 Ozempic better than insulin in lowering the risk of certain cancers: studyThe study included 1.65 million people with Type 2 diabetes who were prescribed insulin, metformin or an Ozempic-like drug between March 2005 and November 2018.
Ozempic better than insulin in lowering the risk of certain cancers: studyThe study included 1.65 million people with Type 2 diabetes who were prescribed insulin, metformin or an Ozempic-like drug between March 2005 and November 2018.
Read more »
 Diabetes patients using Ozempic, other treatments instead of insulin have lower cancer risk, study findsType 2 diabetes patients on GLP-1 treatments, including Ozempic, have a lower risk of 10 types of obesity-related cancers compared to those on insulin, according to a new study.
Diabetes patients using Ozempic, other treatments instead of insulin have lower cancer risk, study findsType 2 diabetes patients on GLP-1 treatments, including Ozempic, have a lower risk of 10 types of obesity-related cancers compared to those on insulin, according to a new study.
Read more »
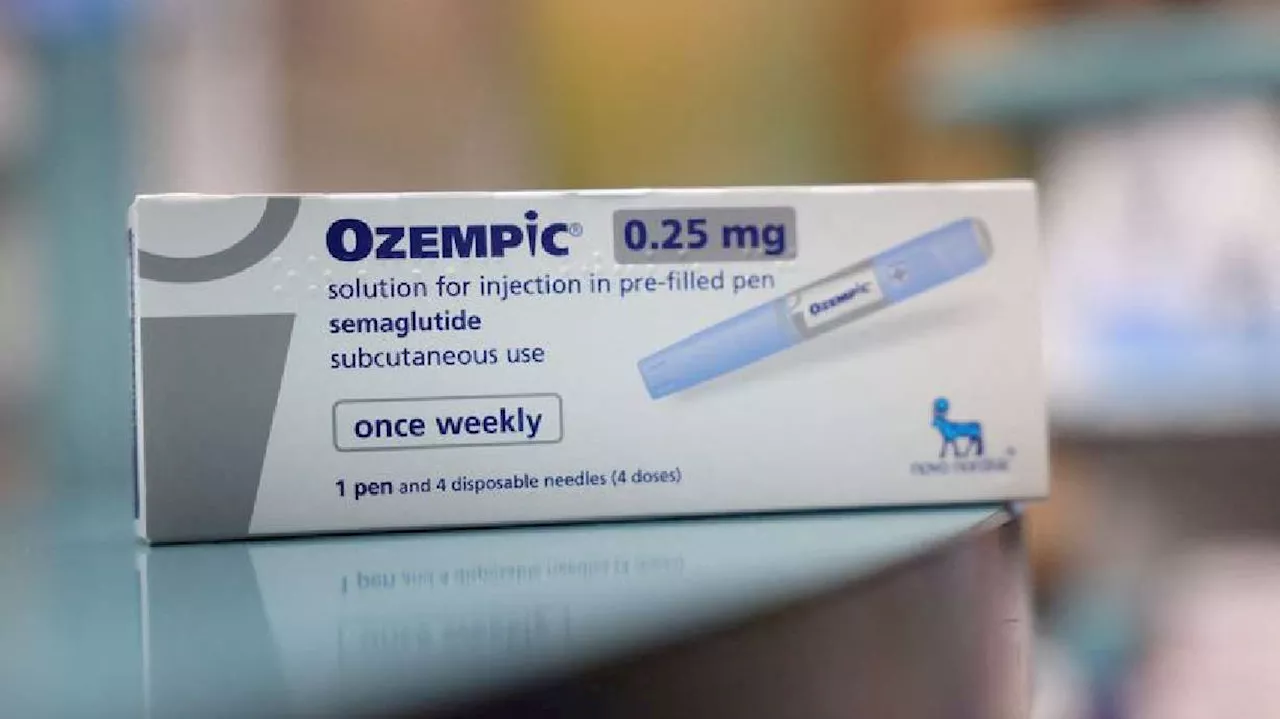 Diabetes patients on GLP-1s instead of insulin have lower cancer risk, study showsPatients with type 2 diabetes taking GLP-1 treatments, which include Ozempic, have a lower chance of developing 10 types of obesity-related cancers than those taking insulin and other diabetes drugs, according to a study published on Friday.
Diabetes patients on GLP-1s instead of insulin have lower cancer risk, study showsPatients with type 2 diabetes taking GLP-1 treatments, which include Ozempic, have a lower chance of developing 10 types of obesity-related cancers than those taking insulin and other diabetes drugs, according to a study published on Friday.
Read more »
