An article published in BMCMedicine reports that separate and combined coffee and tea consumption were inversely associated with all-cause and cause-specific mortality.
]. Body mass index was derived from physical measurement and calculated by dividing weight over height squared. General health status was categorized as excellent, good, fair, and poor. Information on chronic diseases was collected from touchscreen questionnaires, medical examinations, and hospital inpatient records.Mortality information was obtained from death certificates, which were provided by the NHS Information Centre and the NHS Central Register Scotland for the date of death.
]. In our analysis, the null hypothesis was rejected and concluded that there was a nonlinear relationship between separate coffee and tea consumption with all-cause mortality and cause-specific mortality. In the spline models, we adjusted for potential confounders including sex, age, ethnicity, education levels, BMI, smoking status, alcohol intake frequency, physical activity, dietary pattern, general health status, hypertension, diabetes, and depression.
In addition, we performed subgroup analyses to assess potential modification effects and determine whether there was any population heterogeneity according to age, sex, BMI, physical activity, smoking status, alcohol intake frequency, dietary pattern, hypertension, diabetes, and depression. The interactions between baseline characteristics and combined coffee and tea consumption were examined using the likelihood ratio test .Additional analyses were further conducted.
In total, 498,158 participants age: 58 [50-63]; 54% female) were included in this analysis. The proportion of < 1–2 cups/day of coffee and 2–4 cups/day of tea were 46.1% (
United States Latest News, United States Headlines
Similar News:You can also read news stories similar to this one that we have collected from other news sources.
 Call for Papers! Introducing BMC Cancer’s New Collection: Advances in pre-clinical cancer models - BMC Series blogBMC Cancer is calling for submissions to our Collection on novel in vitro and in vivo cancer models, guest edited by Prof. Ryan C. Fields (Washington University School of Medicine in St. Louis, USA) and Dr. Anna Golebiewska (Luxembourg Institute of Health, Luxembourg).
Call for Papers! Introducing BMC Cancer’s New Collection: Advances in pre-clinical cancer models - BMC Series blogBMC Cancer is calling for submissions to our Collection on novel in vitro and in vivo cancer models, guest edited by Prof. Ryan C. Fields (Washington University School of Medicine in St. Louis, USA) and Dr. Anna Golebiewska (Luxembourg Institute of Health, Luxembourg).
Read more »
 Prednisolone does not improve olfactory function after COVID-19: a randomized, double-blind, placebo-controlled trial - BMC MedicineBackground Prednisolone has been suggested as a treatment for olfactory disorders after COVID-19, but evidence is scarce. Hence, we aimed to determine the efficacy of a short oral prednisolone treatment on patients with persistent olfactory disorders after COVID-19. Methods We performed a randomized, double-blind, placebo-controlled, single-centered trial in the Netherlands. Patients were included if they were | 18 years old and if they had persistent (| 4 weeks) olfactory disorders within 12 weeks after a confirmed COVID-19 test. The treatment group received oral prednisolone 40 mg once daily for 10 days and the placebo group received matching placebo. In addition, all patients performed olfactory training. The primary outcome was the objective olfactory function on Sniffin’ Sticks Test (SST) 12 weeks after the start of treatment, measured in Threshold-Discrimination-Identification (TDI) score. Secondary outcomes were objective gustatory function assessed by the Taste Strip Test (TST) and subjective self-reported outcomes on questionnaires about olfactory, gustatory and trigeminal function, quality of life, and nasal symptoms. The CONSORT 2010 guideline was performed. Results Between November 2021 and February 2022, we included 115 eligible patients, randomly assigned to the treatment (n = 58) or placebo group (n = 57). No difference in olfactory function between groups was obtained after 12 weeks. Median TDI score on SST was 26.8 (IQR 23.6–29.3) in the placebo group and 28.8 (IQR 24.0–30.9) in the prednisolone group, with a median difference of 2.0 (95% CI 0.75 to 1.5). There was similar improvement on olfactory function in both groups after 12 weeks. Furthermore, on secondary outcomes, we obtained no differences between groups. Conclusions This trial shows that prednisolone does not improve olfactory function after COVID-19. Therefore, we recommend not prescribing prednisolone for patients with persistent olfactory disorders after COVID-19. Trial registration Thi
Prednisolone does not improve olfactory function after COVID-19: a randomized, double-blind, placebo-controlled trial - BMC MedicineBackground Prednisolone has been suggested as a treatment for olfactory disorders after COVID-19, but evidence is scarce. Hence, we aimed to determine the efficacy of a short oral prednisolone treatment on patients with persistent olfactory disorders after COVID-19. Methods We performed a randomized, double-blind, placebo-controlled, single-centered trial in the Netherlands. Patients were included if they were | 18 years old and if they had persistent (| 4 weeks) olfactory disorders within 12 weeks after a confirmed COVID-19 test. The treatment group received oral prednisolone 40 mg once daily for 10 days and the placebo group received matching placebo. In addition, all patients performed olfactory training. The primary outcome was the objective olfactory function on Sniffin’ Sticks Test (SST) 12 weeks after the start of treatment, measured in Threshold-Discrimination-Identification (TDI) score. Secondary outcomes were objective gustatory function assessed by the Taste Strip Test (TST) and subjective self-reported outcomes on questionnaires about olfactory, gustatory and trigeminal function, quality of life, and nasal symptoms. The CONSORT 2010 guideline was performed. Results Between November 2021 and February 2022, we included 115 eligible patients, randomly assigned to the treatment (n = 58) or placebo group (n = 57). No difference in olfactory function between groups was obtained after 12 weeks. Median TDI score on SST was 26.8 (IQR 23.6–29.3) in the placebo group and 28.8 (IQR 24.0–30.9) in the prednisolone group, with a median difference of 2.0 (95% CI 0.75 to 1.5). There was similar improvement on olfactory function in both groups after 12 weeks. Furthermore, on secondary outcomes, we obtained no differences between groups. Conclusions This trial shows that prednisolone does not improve olfactory function after COVID-19. Therefore, we recommend not prescribing prednisolone for patients with persistent olfactory disorders after COVID-19. Trial registration Thi
Read more »
 Wellcome Collection closes 'racist, sexist and ableist' Medicine Man displayThe Wellcome Collection says its Medicine Man display will end on Sunday after a 15-year run.
Wellcome Collection closes 'racist, sexist and ableist' Medicine Man displayThe Wellcome Collection says its Medicine Man display will end on Sunday after a 15-year run.
Read more »
 Medicine Man display: Wellcome Collection museum in London shuts 'racist and sexist' medical history exhibitionThe Wellcome Collection's display, called Medicine Man, includes objects relating to sex, birth and death, and anatomical models in wood, ivory and wax dating back to the 17th century.
Medicine Man display: Wellcome Collection museum in London shuts 'racist and sexist' medical history exhibitionThe Wellcome Collection's display, called Medicine Man, includes objects relating to sex, birth and death, and anatomical models in wood, ivory and wax dating back to the 17th century.
Read more »
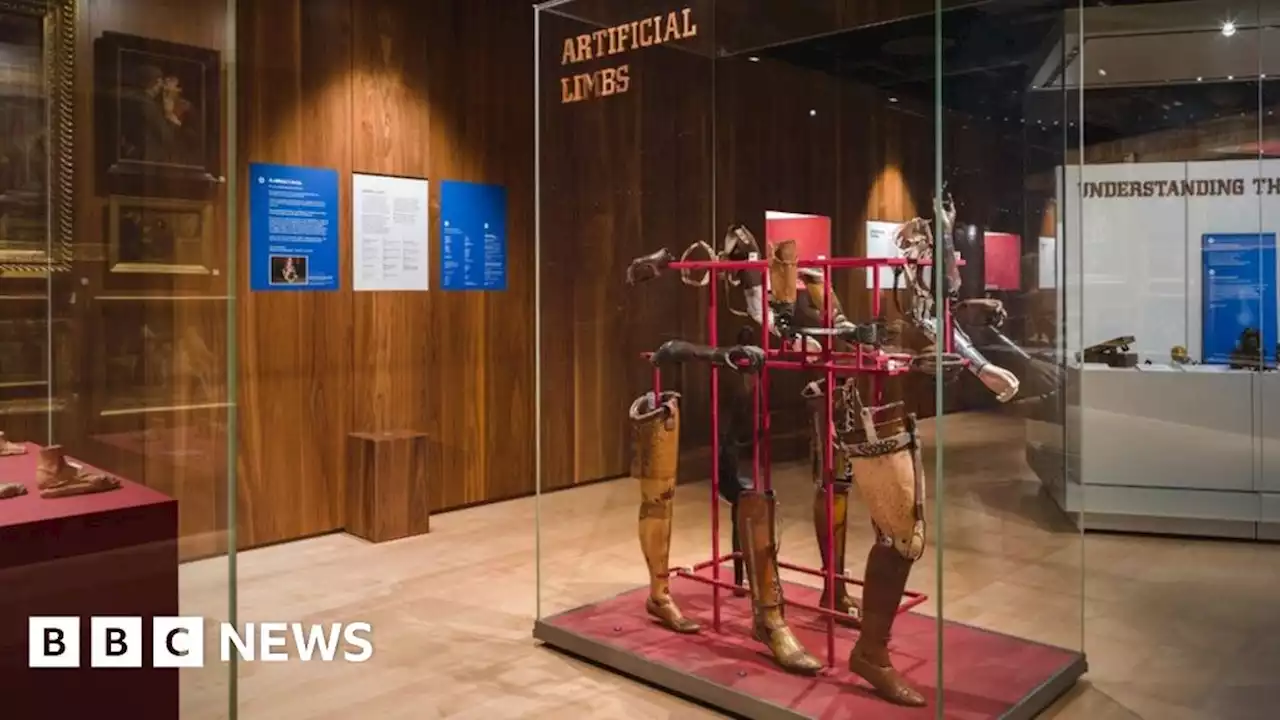 Wellcome Collection closes 'racist, sexist and ableist' Medicine Man displayThe Wellcome Collection says its Medicine Man display will end on Sunday after a 15-year run.
Wellcome Collection closes 'racist, sexist and ableist' Medicine Man displayThe Wellcome Collection says its Medicine Man display will end on Sunday after a 15-year run.
Read more »
 Use of antibiotics and risk of type 2 diabetes, overweight and obesity: the Cardiovascular Risk in Young Finns Study and the national FINRISK study - BMC Endocrine DisordersPurpose To investigate whether exposure to systemic antibiotics influences the risk of developing type 2 diabetes and overweight/obesity. Methods The study sample comprised 2209 (110 with incident diabetes) participants from the population-based Cardiovascular Risk in Young Finns Study (YFS) aged 24–39 years in 2001. The exposure was national linked register data on purchased antibiotic courses between 1993 and 2001. Clinical examinations including BMI were conducted in 2001, 2007 and 2011. Participants with prevalent diabetes in 2001 were excluded. Data on type 2 diabetes was also obtained from two national registers until 2017. Data from four population-based National FINRISK studies were used for replication (N = 24,674, 1866 with incident diabetes). Results Prior antibiotic exposure (| 5 versus 0–1 antibiotic courses) was associated with subsequent type 2 diabetes in both YFS (OR 2.29; 95%CI 1.33–3.96) and FINRISK (HR 1.73; 95%CI 1.51–1.99). An increased risk for type 2 diabetes was observed in YFS (OR 1.043; 95%CI 1.013–1.074) and FINRISK (HR 1.022; 95%CI 1.016–1.029) per course. Exposure to antibiotics increased the risk of overweight/obesity (BMI | 25 kg/m2) after a 10-year follow-up in YFS (OR 1.043; 95%CI 1.019–1.068) and in FINRISK (OR 1.023; 95%CI 1.018–1.029) at baseline per antibiotic course. Adjustments for confounders from early life in YFS and at baseline in FINRISK, including BMI, socioeconomic status, smoking, insulin, blood pressure, and physical activity, did not appreciably alter the findings. Conclusion Our results show that exposure to antibiotics was associated with increased risk for future type 2 diabetes and overweight/obesity and support judicious antibiotic prescribing.
Use of antibiotics and risk of type 2 diabetes, overweight and obesity: the Cardiovascular Risk in Young Finns Study and the national FINRISK study - BMC Endocrine DisordersPurpose To investigate whether exposure to systemic antibiotics influences the risk of developing type 2 diabetes and overweight/obesity. Methods The study sample comprised 2209 (110 with incident diabetes) participants from the population-based Cardiovascular Risk in Young Finns Study (YFS) aged 24–39 years in 2001. The exposure was national linked register data on purchased antibiotic courses between 1993 and 2001. Clinical examinations including BMI were conducted in 2001, 2007 and 2011. Participants with prevalent diabetes in 2001 were excluded. Data on type 2 diabetes was also obtained from two national registers until 2017. Data from four population-based National FINRISK studies were used for replication (N = 24,674, 1866 with incident diabetes). Results Prior antibiotic exposure (| 5 versus 0–1 antibiotic courses) was associated with subsequent type 2 diabetes in both YFS (OR 2.29; 95%CI 1.33–3.96) and FINRISK (HR 1.73; 95%CI 1.51–1.99). An increased risk for type 2 diabetes was observed in YFS (OR 1.043; 95%CI 1.013–1.074) and FINRISK (HR 1.022; 95%CI 1.016–1.029) per course. Exposure to antibiotics increased the risk of overweight/obesity (BMI | 25 kg/m2) after a 10-year follow-up in YFS (OR 1.043; 95%CI 1.019–1.068) and in FINRISK (OR 1.023; 95%CI 1.018–1.029) at baseline per antibiotic course. Adjustments for confounders from early life in YFS and at baseline in FINRISK, including BMI, socioeconomic status, smoking, insulin, blood pressure, and physical activity, did not appreciably alter the findings. Conclusion Our results show that exposure to antibiotics was associated with increased risk for future type 2 diabetes and overweight/obesity and support judicious antibiotic prescribing.
Read more »