Dr. Farzon Nahvi spent the first few months of the pandemic as an emergency room physician in Manhattan. He talks about trying to improvise treatments during that time. His new book is Code Gray.
Dr. Farzon Nahvi spent the first few months of the pandemic as an emergency room physician in Manhattan. He talks about trying to improvise treatments during that time. His new book isThis is FRESH AIR. I'm Dave Davies, in for Terry Gross. In the first year of the pandemic, more than 3,600 American health care workers died after being infected with the COVID-19 virus.
It felt in that moment that we were one step ahead of all the guidance we were getting because we were there on the ground experiencing this. And then the guidance we would get would often come one or two weeks later. So we were really relying on each other for everything - what to do, how to treat people, what our situations were like in our different hospitals. If our family members got sick, we would ask each other to check up on each other's family members.
And you look back and you say, hey, is that really as I remembered it? Was it really as crazy? And it was. But it was just so brief that it's hard to look back and appreciate it for that dramatic episode that it really was. DAVIES: You mentioned a lot of colleagues for the first time sought therapy. Did you seek help yourself?
NAHVI: You know, there was just a lot of anger at that time. I'm not necessarily an angry person by nature. That's not my go-to. But I just remember being kind of uncharacteristically angry during that time period and having someone there to help me through that, I think was extraordinarily valuable.
NAHVI: Well, yeah, like you said, just from hearing that report, it's clear that she's died, and there's going to be no successful chance at bringing her back. And yet we do what we always do, which is that we prepare to do everything in full capacity. You always worry that there's some sort of miscommunication or something else might have happened that we didn't really catch word of 'cause the communications in the pre-hospital setting, they can be a little rocky.
DAVIES: You know, as you describe what happens here - and this is a conversation that moves as a thread throughout the book while you discuss related topics. But it's interesting that you tell us in the book that there's no set standard for how long you continue CPR after you're not getting a pulse. And you and this team - and it's quite a team - really work on this woman. I mean, it's clear at some point that it's not going to be successful.
NAHVI: Yeah. No, I didn't handle it well at all because they teach this stuff in med school and residency but it's all theoretical. The real-life doing it is an entire different level. And in that particular example, I knew the information I had to tell her, and yet I just found myself literally unable to speak the words. Up until that in my whole entire life, I've never had to confirm someone's deepest anxieties and fears.
NAHVI: Well, yeah, absolutely. I had this recognition immediately after I walked away. I just - kind of my mind was reeling, that, oh, geez, I didn't even tell her . And then, I had to have this awkward about-face where I walked back and say, hey, you know, I don't think I actually communicated as well as I could have, and I had to. So those things that I was talking about, those bad things, it does look like you have metastatic cancer.
DAVIES: I'm sure she went on and got, you know, treatment beyond the ER. Do you know what happened with her illness? And generally, when I try to do this, when someone's died, there's not a lot of information that I feel that I need to give in terms of, this is the next step in your process, or this is your treatment. A lot of it is just reassurance for that person that they did the right thing, that the paramedics that took care of the patient on the way to the hospital did the right thing, that, you know, we in the hospital did all of these things.
DAVIES: This is FRESH AIR. I'm Dave Davies, in for Terry Gross. We're speaking with Dr. Farzon Nahvi, an emergency room physician at Concord Hospital in Concord, N.H. He spent the early months of the COVID pandemic on the front lines in emergency rooms in New York City. His new memoir is about his experiences in the ER and his frustrations with American health care. It's called"Code Gray: Death, Life, And Uncertainty in the ER.
NAHVI: When you work in the ER, you kind of get used to every little detail in every little tone of voice. And I remember our beginning of our conversation was normal. She was a little bit hurried. She was helpful, but she wanted to get to know kind of why I was calling. And I told her the name of who I was calling for. And immediately, once she heard that name, she slowed down her cadence. And she took the time to speak with me. She didn't necessarily get kinder.
And I think there's a lot of people out there who say that this kind of compartmentalization and detachment is necessary, that if you get too close to those experiences and take them too seriously that you're going to get too attached and you can't perform your job. But I think that's a misread. I think that's certainly a coping mechanism, but I think it's a poor coping mechanism. I don't think you could pretend to be unaffected by this stuff.
DAVIES: Oh, that's so interesting, you know? I mean, everybody is so busy. They have other tasks to get to. But taking a moment to just acknowledge this pain makes a difference.DAVIES: In the case of the woman who - the 43-year-old woman who had died and, you know, you let the husband sit with the wife's body, and then you spoke to him. And at some point, then you have to put in your notes. I mean, you fill out a death certificate. You put in your notes.
NAHVI: It depends on the hospital I've worked for. I've worked for public hospitals who do have a mission to just take care of people. And no, I don't get that pressure there. But many of the private hospitals I work for, there's a phrase that's called strive to five, meaning try to get that Level 5 billing code, you could say.DAVIES: Let's take another break here. Let me reintroduce you. We are speaking with Farzon Nahvi.
So her chemo - her oncologist wasn't able to see her anymore because she didn't have insurance anymore. So he or she referred this patient to our hospital, which was a public hospital where I was working at the time. She didn't understand that she had to go see an oncologist. So she just came to the emergency room. And I thought there was a misunderstanding.
In the eyes of this legislation, she was stable. So she had cancer, and she was dying, but she was dying slowly. She wasn't dying quickly. So she was technically stable. And it became this kind of horrible thing that I had to explain to her that, yes, you're protected by this law and yes, you have cancer and yes, you're dying, but I can't help you.
What he told me was that people take veterinary antibiotics all the time, and he gets cases reported about that routinely. But when you take dog or cat antibiotics, people usually do fine because they're pills, and they're the right dosage. Whereas fish formulation, it's just highly dense, highly concentrated 'cause you're supposed to dissolve it into a fish tank so that the fish can eventually drink it when they have their water.
United States Latest News, United States Headlines
Similar News:You can also read news stories similar to this one that we have collected from other news sources.
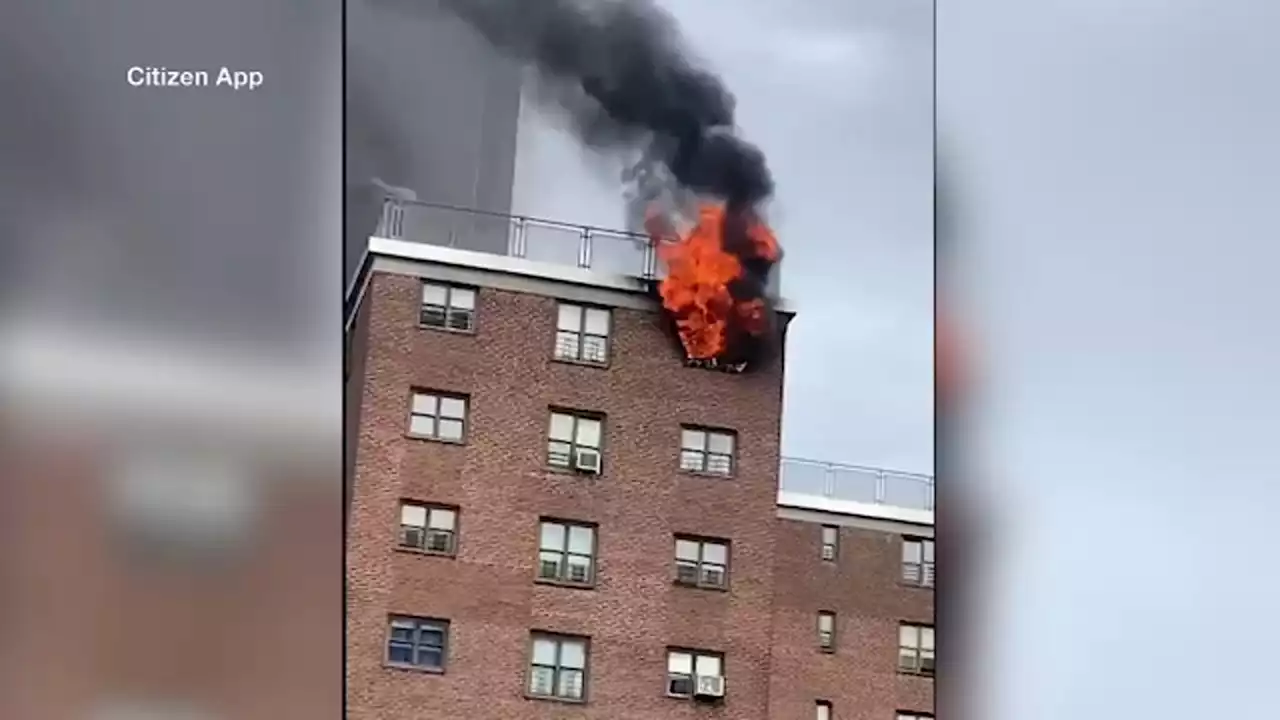 2 injured after fire breaks out at Lower Manhattan high-riseFlames shot through the top floors of a NYCHA complex on St. James Place and Madison Avenue on Sunday afternoon.
2 injured after fire breaks out at Lower Manhattan high-riseFlames shot through the top floors of a NYCHA complex on St. James Place and Madison Avenue on Sunday afternoon.
Read more »
 NYPD vehicles vandalized in Lower ManhattanPolice said they have video of a female vandal in a yellow baseball cap fleeing the scene afterward.
NYPD vehicles vandalized in Lower ManhattanPolice said they have video of a female vandal in a yellow baseball cap fleeing the scene afterward.
Read more »
 Pride Flag Hanging Outside Manhattan Restaurant Set on FireAuthorities say a gay pride flag was intentionally set ablaze outside a Manhattan restaurant in the middle of the night. Firefighters and police responded to Little Prince restaurant in Soho around 1:30 a.m. Monday for reports of a fire. Flames caused some minor damage to the front of the restaurant, but no injuries were reported. “Hate in SoHo: Last night…
Pride Flag Hanging Outside Manhattan Restaurant Set on FireAuthorities say a gay pride flag was intentionally set ablaze outside a Manhattan restaurant in the middle of the night. Firefighters and police responded to Little Prince restaurant in Soho around 1:30 a.m. Monday for reports of a fire. Flames caused some minor damage to the front of the restaurant, but no injuries were reported. “Hate in SoHo: Last night…
Read more »
 Woman caught on video setting fire to gay pride flag outside Manhattan restaurantNew York City police are searching for the woman seen on video setting fire to a gay pride flag in front of a Manhattan restaurant.
Woman caught on video setting fire to gay pride flag outside Manhattan restaurantNew York City police are searching for the woman seen on video setting fire to a gay pride flag in front of a Manhattan restaurant.
Read more »
 Woman caught on video setting fire to gay pride flag outside Manhattan restaurantNEW YORK — New York City police are searching for the woman seen on video setting fire to a gay pride flag in front of a Manhattan restaurant.
Woman caught on video setting fire to gay pride flag outside Manhattan restaurantNEW YORK — New York City police are searching for the woman seen on video setting fire to a gay pride flag in front of a Manhattan restaurant.
Read more »
